What is a Morel Lavallee Lesion?
A Morel Lavallee Lesion is a closed soft-tissue degloving injury in which an extensive section of skin is completely torn off from the underlying tissue of the affected part. A degloving injury in the form of Morel Lavallee Lesion refers to an avulsion or surface trauma where the outermost layer of the skin has been completely cut off in the form of “removing a glove.”
Morel Lavallée Lesions have derived their name from French physician Maurice Morel-Lavalee who first described the condition in 1853.
What is a Hematoma?
A Hematoma is a collection of blood outside blood vessels caused by injury or during a surgical procedure. Hematoma is a common phenomenon and is observed immediately after bruises or falls. Sometimes, the problem can result from medical conditions as well.
Medically Hematoma is called ecchymosis and can occur anywhere in the body. Because of their nature of occurrence, especially in the soft tissues, morel lavallee lesions and hematomas are sometimes confused as similar, which is not the case.
Below mentioned are some differentiating features between Hematomas and Morel Lavallee Lesions
Differentiating Features between Morel Lavallee Lesion and Hematoma
Occurrence Point
Morel Lavallee Lesions occur in the top layers of skin and tissues and mostly affect the legs.
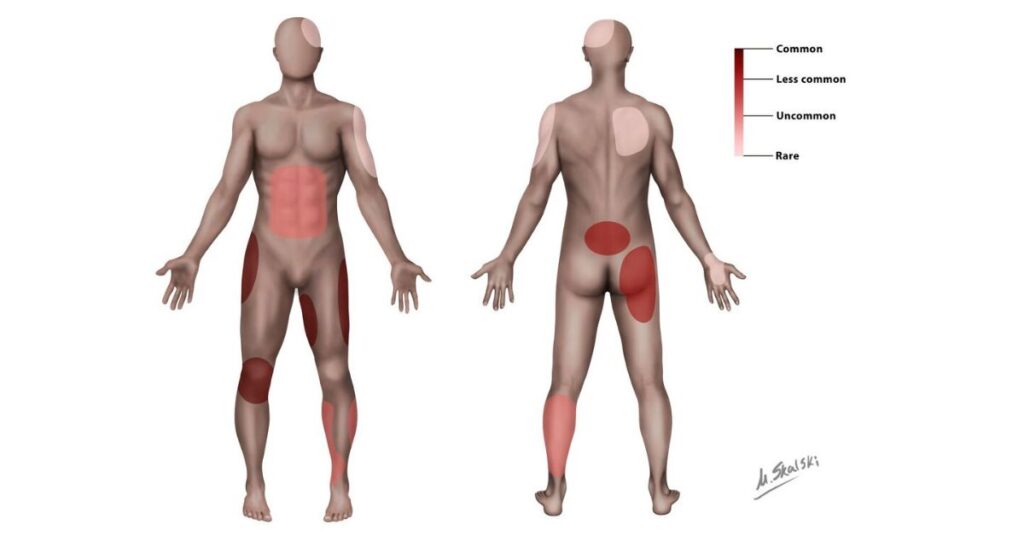
Hematomas can occur in any area of the system with blood vessels or capillaries. When near the skin or subcutaneous regions, they appear more superficially than a Morel Lavallee Lesion.
Incidence
Morel Lavallee Lesion is a rare phenomenon with a prevalence of approximately 1.56%.
A study conducted on 3279 trauma patients over five months showed only 1% (33) MLLs in trauma patients with underlying fractures and 0.56%(18).
The incidence of Hematoma depends on its site of occurrence. For example, Superficial hematomas are very common, impacting most people with injuries. Subdural Hematomas, or clotting of blood vessels between the skull and the brain, have an incidence of 14.7 out of 100,000 individuals in the U.S. Epidural Hematoma in people with head injuries is approximately 2-15%.
Physiology
Morel Lavallee Lesions are traumatic closed degloving injuries occurring in the subcutaneous plane or skin layer just above the muscle plane and result in the accumulation of hemolymph with necrotic fat.
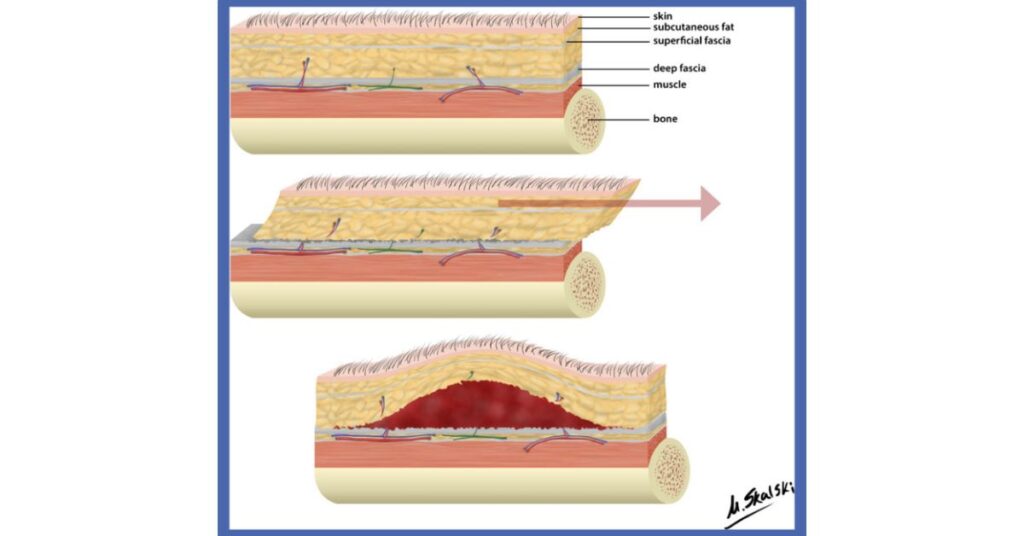
Hematoma occurs when the blood vessels in an area start leaking and pooling in the surrounding tissues.
Causes
Morel Lavallee Lesions can occur because of
- Accidents involving industrial or farm equipment
- Construction accidents
- Car or Motorcycle accidents
- Animal Bites
- Falling from heights
Hematomas can occur because of
- Traumatic conditions
- Effect of medications
- Viral Infections
- Aneurysms
- Orthopedic complications like fractures
Classification
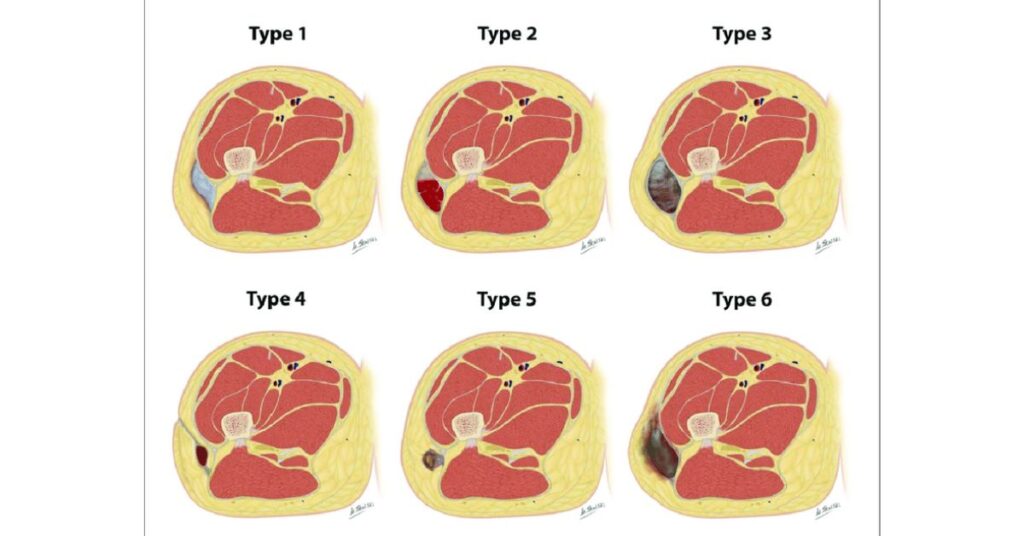
Types of Morel Lavallee Lesions
Type 1 – laminar shaped and seroma like
Type 2 – oval shaped resembling a subacute hematoma
Type 3 – oval shaped resembling chronic organizing hematoma
Type 4 – linear, like a closed laceration
Type 5 – pseudo nodular with a round shape
Type 6 – infected with a thick capsule and peripheral enhancement
Classification of Hematoma
Based on its location, a Hematoma can be
Subcutaneous – under the skin
Subungual – under the toenails
Retroperitoneal – inside the abdominal cavity without involving the organs
Hepatic – in the liver
Splenic – in the spleen
Intracranial – between the skull and lining of the brain
Subdural – between the brain tissue and the internal lining of the brain
Symptoms
The most common symptoms of Morel Lavallee Lesions are
- Pain
- Swelling
- Palpable fluctuant collection over the injured area
- Hypoesthesia
The symptoms of Hematoma vary as per the area of its occurrence. E.g.-
- Subcutaneous hematoma results in red swelling, purplish bruises, a warm sensation of pain
- Subungual hematoma results in discoloration of the nail
- Intracranial Hematoma leads to slurred speech, vomiting, dizziness, unequal pupil size
- Intracranial Hematoma leads to slurred speech, vomiting, dizziness, unequal pupil size
External appearance
Morel lavallee Lesion
Intramuscular Hematoma

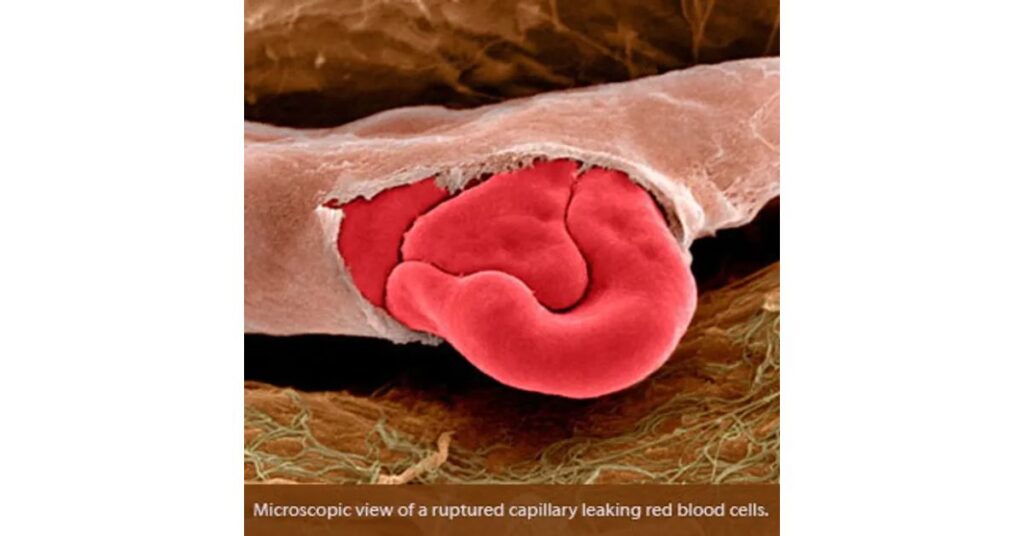
Impact on blood vessels
A Morel Lavallee Lesion results in proliferative damage to capillaries and blood vessels in the affected area.
Hematoma partially damages the blood vessels resulting in seepage of blood to the surrounding areas. But it does not destroy them.
Microscopic Appearance
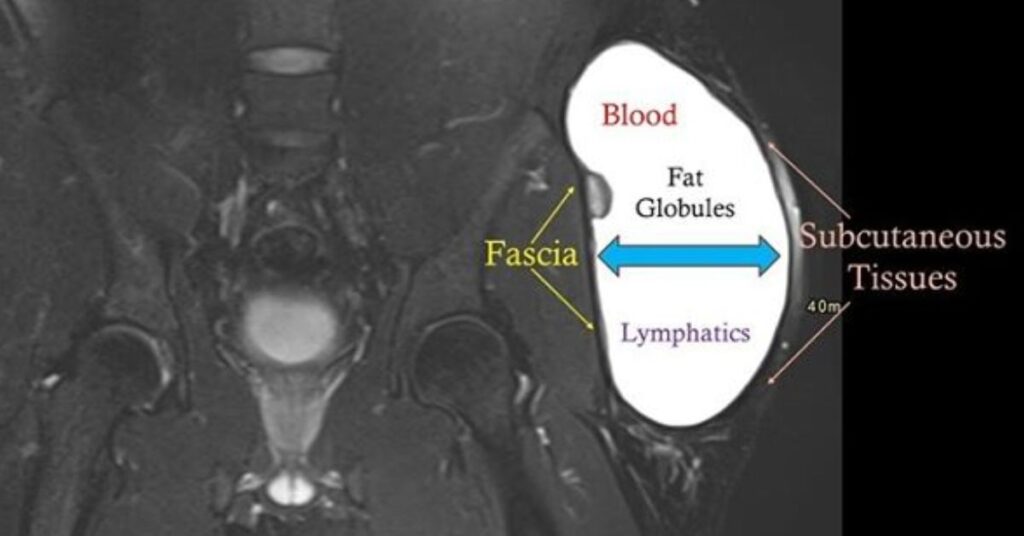
Image 1 – Morel Lavallee Lesion
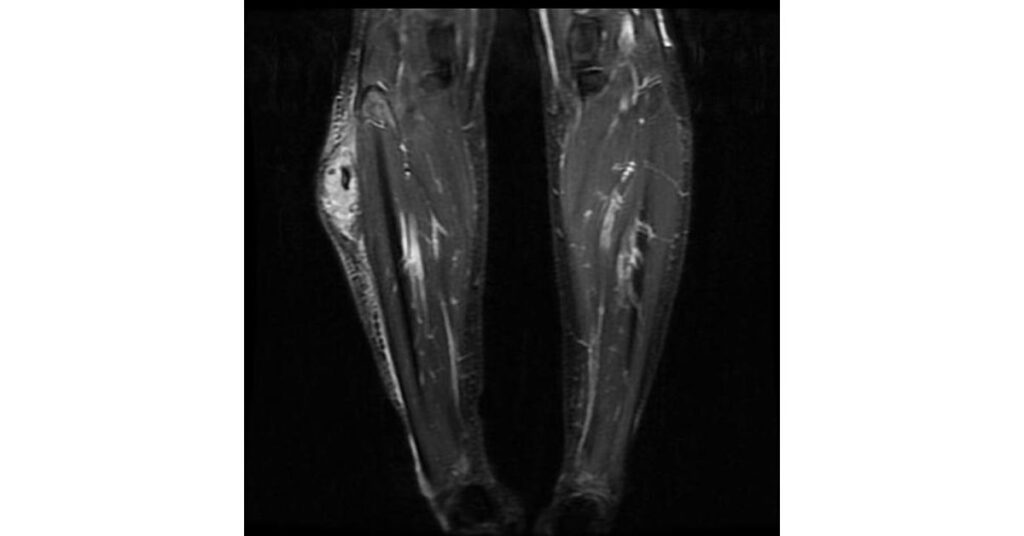
Image 2 – Hematoma
Impact on tissue
Morel Lavallee Lesions damage the tissue and lead to their necrosis in severe conditions because of disruption of blood vessels caused by the impact.
Whether or not a hematoma can impact the tissue depends on its position and how promptly it is treated. Studies have shown that intracranial and traumatic subcutaneous Hematoma can cause significant tissue damage if left untreated. Hematoma under the nails though painful, does not cause tissue damage.
Diagnostic Methods
Diagnosis of Morel Lavallee Lesion is based on the history of the patient, physical examination conducted by a medical expert, and imaging methods. Some of the diagnostic procedures used are
Ultrasound – that helps diagnose the fluid mass
MRI – that helps in differentiating from hematomas
CT Scans
Diagnosis of Hematoma is conducted through physical examination and CT scans.
Treatment Method
Morel Lavallee Lesions are notoriously challenging to treat because of the secondary infections that develop over them. Some of the chief treatment options for MLLs are
- Sclerosing agents like Erythromycin, Bleomycin, Absolute Alcohol
- Surgical interventions like Skin Grafting or Local Flap-Based Reconstruction
Hematomas, especially when of a superficial origin, are self-treatable and don’t require medical intervention. Treatment for hematomas include
- RICE Method ( Rest, Ice, Compression, and Elevation )
- Over The Counter painkillers, if required
- Occasionally, Surgical intervention if it impacts the vital organs
Differential Diagnosis
Differential Diagnosis of Morel Lavallee Lesion includes
- Seroma
- Hematoma
- ‘Soft Tissue Malignancy
- Bursitis or inflammation of the protective covering of the bones
- Abscess
Differential Diagnosis of a Hematoma depends on its area of occurrence. For Eg-
- Subcutaneous Hematoma is differentially diagnosed with a bruise
- Subdural Hematoma in the brain is differentially diagnosed with a brain tumor, hemorrhagic stroke, and neurosyphilis
- Spinal Hematoma is differentially diagnosed with Spondylitis
Tabular Representation
| Characteristics | Morel Lavallee Lesion | Hematoma |
| Definition | Closed soft-tissue degloving injury | Collection of blood outside of blood vessels |
| Occurrence | Top layers of skin | Anywhere in the system, including skin |
| Incidence | Rare | Variable factor |
| Physiology | Formed in a subcutaneous plane through the destruction of skin and capillaries | Formed because of leakage of blood vessels |
| Causative Factors | Trauma | Traumatic, systemic, and surgical factors |
| Classification | Five subcategories based on skin affection | Classification based on the area of occurrence |
| Symptom | Pain, swelling, fluctual collection | It depends on which area of the system is impacted |
| Impact on blood vessels | Completely destroyed | Leal but are not destroyed |
| Impact on tissue | Tissue damage throughout the affected area | Tissue damage may occur in some cases |
| Diagnosis | Physical examination, MRI. CT scan | Self Diagnosis. Physical examination with occ MRI/CT scan |
| Treatment | Surgical or systemic intervention | Self-treatment, OTC painkiller, systemic intervention |
| Differential Diagnosis | Seroma, Hematoma | It depends on the area of the Hematoma |
Reference:
- rxlist.com/hematoma/drugs-condition.htm
- tgh.org/institutes-and-services/conditions/degloving-injuries#:~:text=A%20degloving%20injury%20is%20a,frequently%20associated%20with%20underlying%20fractures.
- emedicine.medscape.com/article/1137065-overview
- radiopaedia.org/articles/mellado-bencardino-classification-of-morel-lavallee-lesions-1#:~:text=type%20I%3A%20laminar%2Dshaped%20and,capsule%20and%20internal%2Fperipheral%20enhancement
- ncbi.nlm.nih.gov/books/NBK574532/
- ncbi.nlm.nih.gov/pmc/articles/PMC8500644/